Posted On April 25, 2022
Automating Prior Authorization to Optimize Revenue Cycle management (RCM)
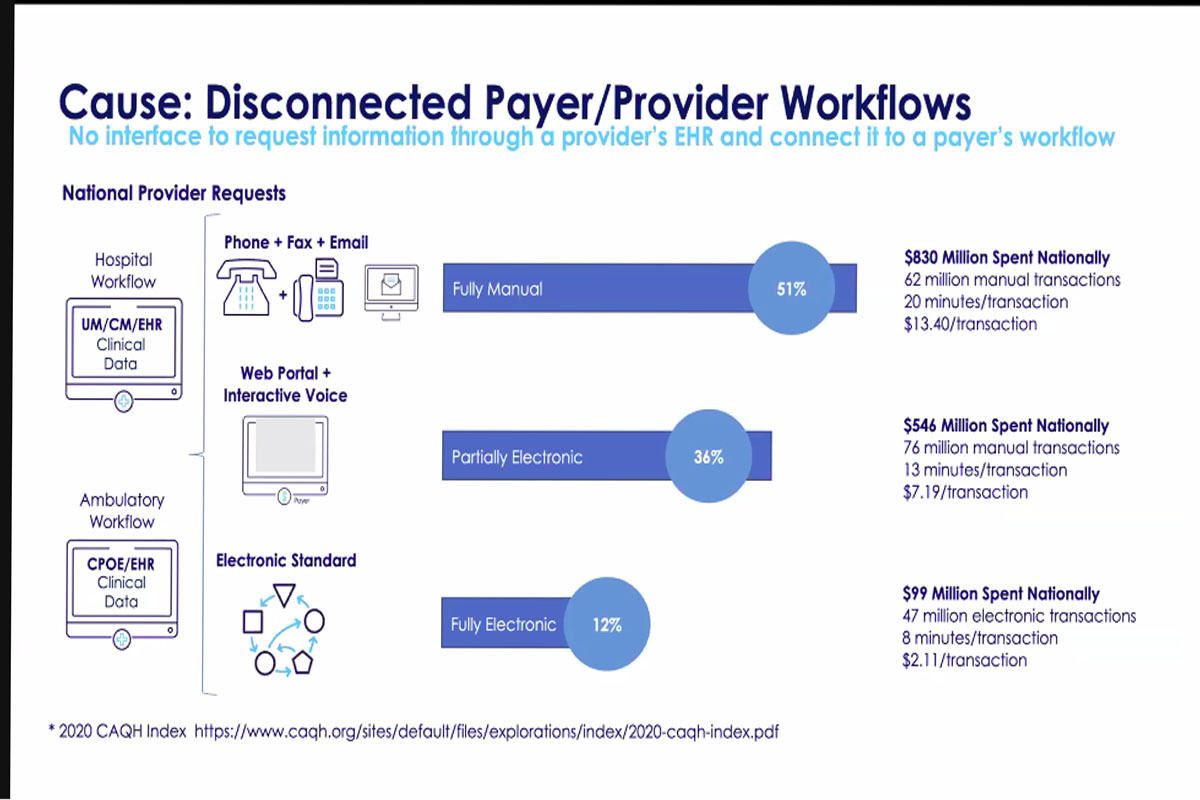
Prior authorization is an expensive and complex process, and the primary reason for claim denials for Providers is an inability to implement the proper process and documentation during the prior authorization phase. Approximately 90% of Prior Authorisations (PA) are still handled offline via IVR, mail, and phone calls. Only one-fifth of the 182 million transactions were automated between 2016 and 2020. Prior authorization has a lot of potential for automation, but it still uses old-school claim processing methods. The transition from manual to digital communication channels should be centered on market needs for providers and payers, as well as technology/capability, and should be followed by its outcomes.
Electronic authorizations are the need of the day considering the transactional cost associated and the number of denials associated with manual authorization. To guide/recommend our clients on the same, we need to be up to date on the relevant skillset and technologies paving the way for data interoperability in healthcare. Interoperability based on HL7, FHIR, and CDS Hooks will be the ultimate solution for optimizing clinic workflow, reducing denials, and reducing operation/administrative costs.
Currently, providers are employing people to manually enter information from EHR to the claim portals, which results in high operational costs. If you don’t capture accurate demographics, you’ll get incorrect eligibility and benefits, making it difficult to be “accurate” in your authorization. Auth rules are embedded in the contract between the employee and the insurance carrier, so there is a lot at stake.
Implementing the EDI 278 solution, which allows providers to submit all prior authorization requests to all payers in their network, opens up a world of possibilities and opportunities. The interoperability market is expected to pick up steam in the coming years as advancements in AI/ML/RPA and data interoperability standards significantly improve PA, patient-provider data structuring, and claim management.
The future trajectory of standard adoption will be determined by the following criteria: who are you, do I allow this, is it relevant and is it clinically necessary. Processes such as Coverage Requirements Discovery (CRD), Documentation Templates and Rules (DTR), Prior Authorization Support (PAS), and, Implementation Guides (IGs) work together to automate the submission of required documentation and/or prior authorization from EHR and payer systems. Process enablers such as the Da Vinci and X12 projects enable payers, health systems, and other industry participants to identify and enumerate clinical and administrative data management and sharing among industry partners. Healthcare Interoperability service providers, in collaboration with HL7 International, are bringing payers, providers, patients, healthcare technology vendors, and all the other stakeholders together to work in a collaborative ecosystem.